Crisis Services Prove to Be Life-Saving Option
The glass and metal doorway at Monarch’s Lumberton Facility-Based Crisis Center, 207 West 29th Street, has been witness to all walks of life crossing the threshold. They walk through with a hope to receive support to overcome a substance use disorder (SUD) or a mental health crisis, or at times, both.
Lumberton FBC services are two-fold: one that offers a non-hospital, medical detox program for individuals with SUD issues and the second that treats people experiencing a mental health crisis, at times in combination with an SUD. For some, the detox process can be in depth with associated withdrawal side effects however a number of substances do not have physical side effects. The typical length of stay at the Lumberton FBC is seven to 14 days.
For People Seeking Recovery, Rock Bottom is Different for Everyone
Lumberton FBC’s Behavioral Health Therapist Mary Locklear, MS, LCMHC-S, LCAS, CCS, says people seeking services are “vulnerable, discouraged, desperate, physically sick, hungry, tired, reporting feelings of shame and rejection.” The staff work together, Mary explains, to assist the person seeking services so that their end result is “leaving the program with some sense of hope, some sense of direction, and encouragement that they can try again.”
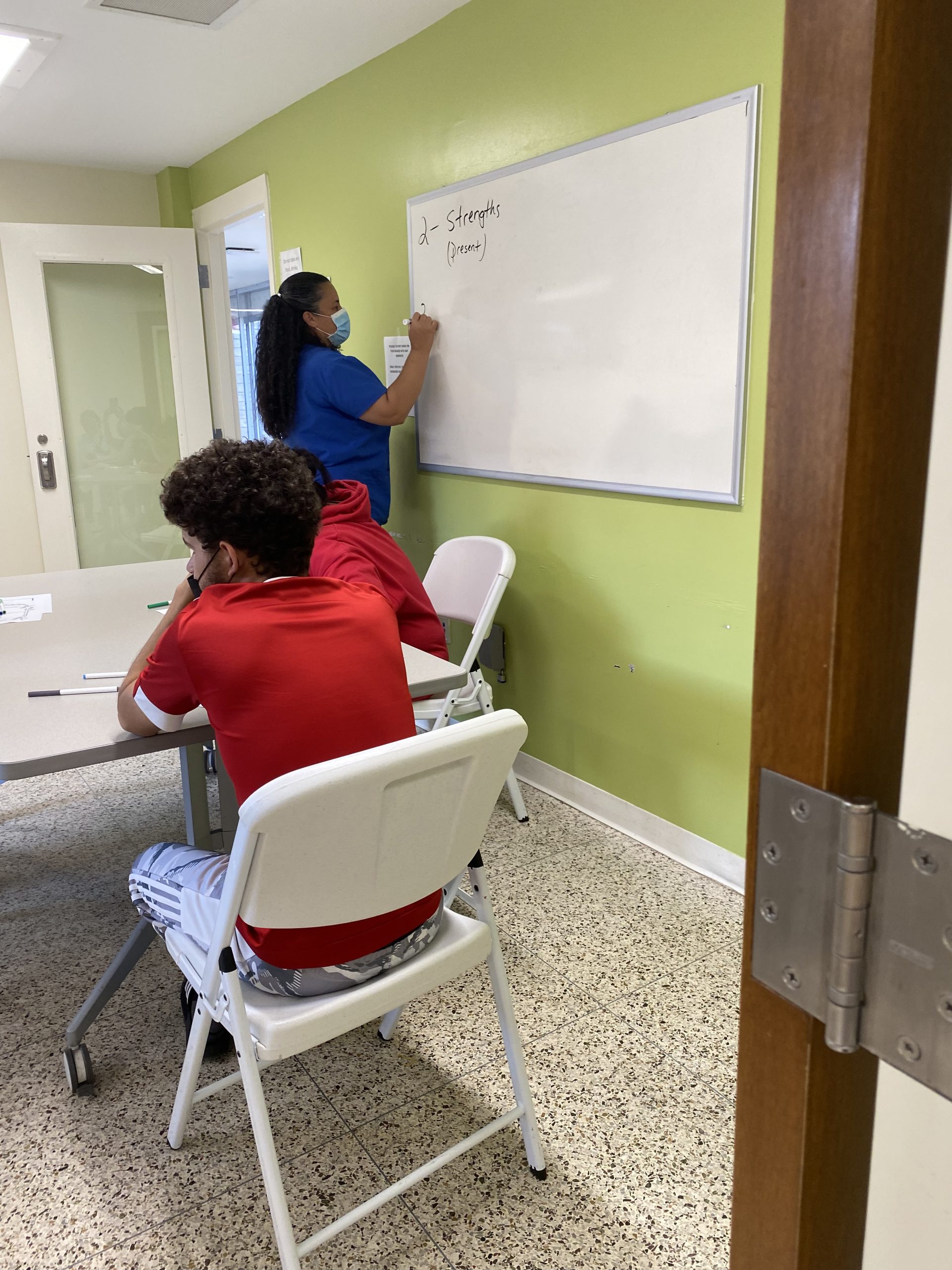
Team Collaboration Assists in Treatment
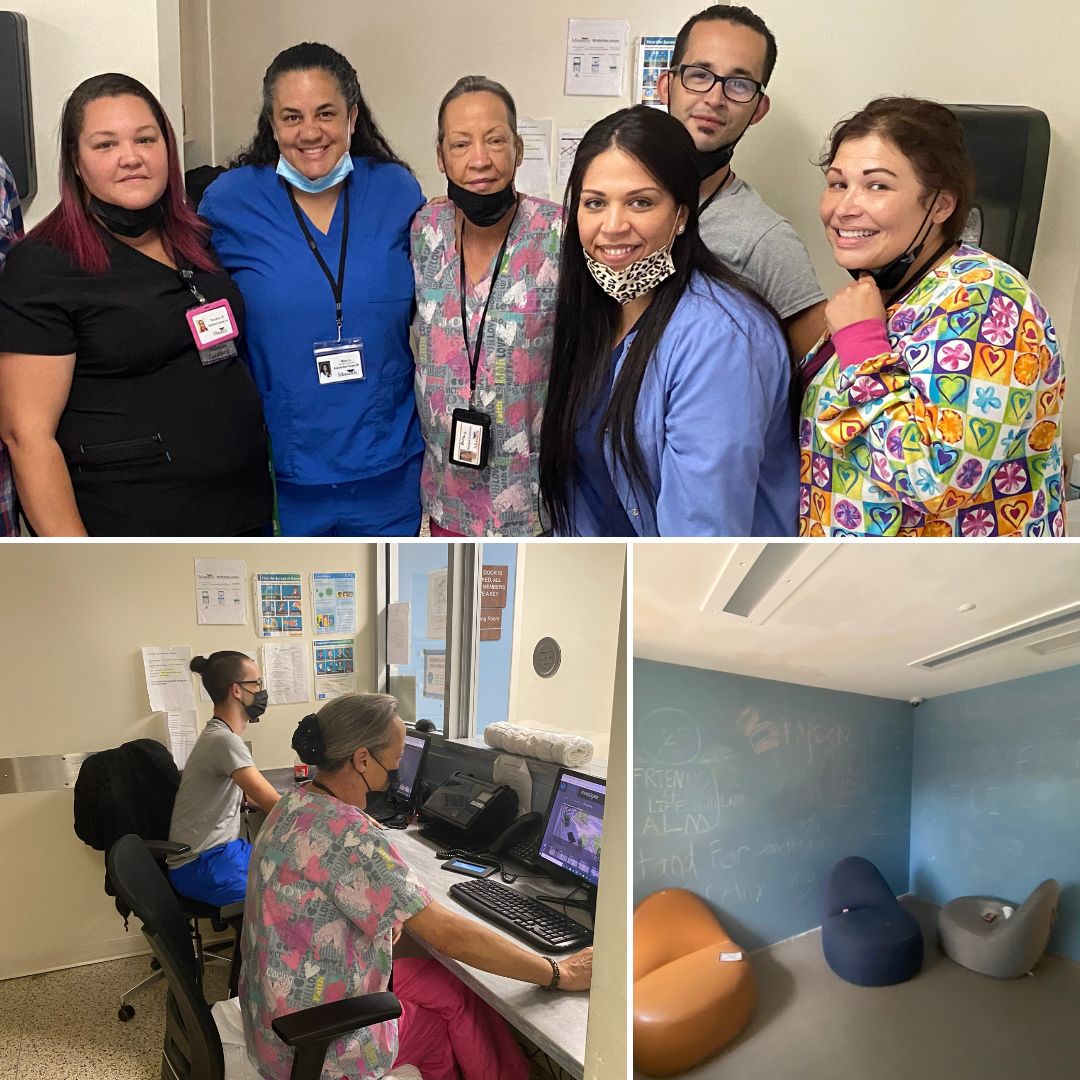
Monarch’s team of staff at the FBC has seen hundreds of people served. Their goal is to help stabilize a person with medication and therapy and make sure they have a discharge plan in place. For someone who has an SUD, that follow up plan is an important step in ensuring they are safe once they leave the FBC.
Mary and other staff at the FBC agree that working together offers the best options for people served starting with daily team treatment meetings bringing together nurses, therapists, nurse practitioner, qualified mental health professionals and behavioral technicians. The team works collectively to share insight and provide input about each person they support. A provider may pick up on something that a therapist did not see. The nurses and qualified professionals all interact with people in different ways and may pick up on different things. Together, they can help create the best outcome for the person receiving care.
Trends in Substance Use
Mary explains that today’s street drugs are lethal, unlike 25 years ago when crack cocaine or powder cocaine were the most dangerous drugs. Heroin, opioids and fentanyl have changed the SUD landscape.
Earlier this year, the North Carolina Department of Health and Human Services announced that an average of nine North Carolinians died each day from a drug overdose in 2020, a 40 percent increase from the previous year translating to an increase of 1,000 lives from 2,352 in 2019 to 3,304 in 2020.
The report also states that studies indicate that “the increase in overdose deaths in recent years is driven by illicit opioids, such as heroin and fentanyl.” Statistics indicate that in 2020, more than 70 percent of overdose deaths in the state likely involved illicitly manufactured fentanyl, often in combination with other substances.
“The potency is now amplified to a pharmaceutical grade making the withdrawals harder, risk of overdose increased and the likelihood of the addict’s mortality becoming fatal,” Mary informs. “With today’s street drug strengths, addiction is not a matter of if but when. There are few cocaine only users, even less alcohol abusers, but more of a cocktail mix of uppers and downers such as ecstasy and opioids, or a cocaine and opioids combination.”
Moanrch staff stay up to date with online resources and information from people they serve about what certain drugs are called on the streets.
A Future of Hope
Monarch staff hope that when people leave the FBC they are able to be successful and remain sober as a functioning member of society. That is not a easy thing to do, but staff hope they have given each person the tools to help them get started.
Mary’s wish for the future of the people served is also straightforward: “My hope is that they simply leave better than they came. That the people we serve can feel like they have a choice, feel like someone can relate to them and be willing to accept help from another human being through therapeutic trust.”
Jada McCarthy, RN, says helping people get the care that they need, recover and return to their lives is rewarding, however there is a difficult part of her role. “The most difficult part of my job is seeing them come back. That is the worst part,” she says of seeing them walk back through the doors after having received treatment following a relapse.
Message for People Struggling to Overcome an SUD
People choosing the option to heal from their mental health crisis or addiction is one of the many positives Mary sees. “It is amazing how a group of people bond, groups as small as four people who have never met, different ages, different ethnicities, different cultures and genders. They come together and get to know each other, connect to each other and encourage one another,” she says.
Andrew Palazzola, a person served who spent time at the Lumberton FBC in August, was grateful for the opportunity and had made plans to continue receiving recovery treatment at an inpatient program in Florida. “I feel better. I feel a whole lot better. I feel great. I have been here seven days and everything has been so right, so positive. I have had good on conversations with the qualified professional. They are helping me. Monarch is a beautiful place to come,” he expresses.
Posted on: Friday March 17, 2023